Arthritis is everywhere so it’s easy to underestimate its severity. For many Canadians living with inflammatory rheumatoid arthritis, it can be thoroughly debilitating.
In 2015, Eileen of Vancouver was a new mother in her twenties. If that wasn’t hard enough, she was also experiencing chronic pain and inflammation in her hands, feet, and knees. “I was unable to function,” Eileen says. “Simple tasks like grocery shopping, taking my kid out to play, or making it to work on time became increasingly difficult because of pain, fatigue, consistent fevers, and increasing depression.”
At first, Eileen chalked all this up to post-pregnancy hormones, but her symptoms worsened and she knew she had to seek help. The diagnosis came back unmistakably. Eileen had rheumatoid arthritis. “I was only 29,” she recalls. “I had no clue I could get arthritis so young, or what arthritis really was.”
I had no clue I could get arthritis so young, or what arthritis really was.
Chronic, incurable, and surprisingly common
Rheumatoid arthritis (RA) is an autoimmune disorder that affects about one percent of adult Canadians. The effects on the body are wide-ranging and go well beyond the finger stiffness that many first think of.
“RA is a lot more than joint pain. It’s a systemic illness,” says Dr. Elizabeth Hazel of the McGill University Health Centre’s Rheumatology Division in Montreal. “While the first symptoms may be painful swollen joints, most patients will have associated fatigue, morning stiffness, and may even feel like they have the flu.”
Early intervention makes all the difference
Because RA is a progressive disease that causes irreversible damage, the earlier the diagnosis and treatment, the better the outcome. Though it’s incurable, the right treatment plan can not only slow progression of the disease, but restore quality of life. “Before finding a medication that worked for me, my joints would be on fire,” says Eileen. “Today I still have pain and fatigue, but I can function significantly better, including walking up a flight of stairs or crushing five kilometres on the elliptical several times a week. It took a long time to get here and a lot of different medications, but the relief is worth it.”
That time on the elliptical isn’t just a result of Eileen’s treatment plan, but also part of it. As a systemic disease, RA responds to practical therapy. Medication plays an important role, but so do things like quitting smoking, maintaining a healthy diet, exercising regularly, and taking care of mental wellness.
“It’s important for anyone who is living with RA or any chronic illness to take ownership of their disease,” says Dr. Hazel. “If available, I highly recommend that patients be referred to rehabilitation programs that include sessions in occupational therapy, physiotherapy, nutrition, psychology, social work, and work reorientation.”
Living with RA is a journey, but the first step of that journey is always talking to your health care professional to find the best personalized treatment plan.
From Biologics to Biosimilars: The Art of Equivalence
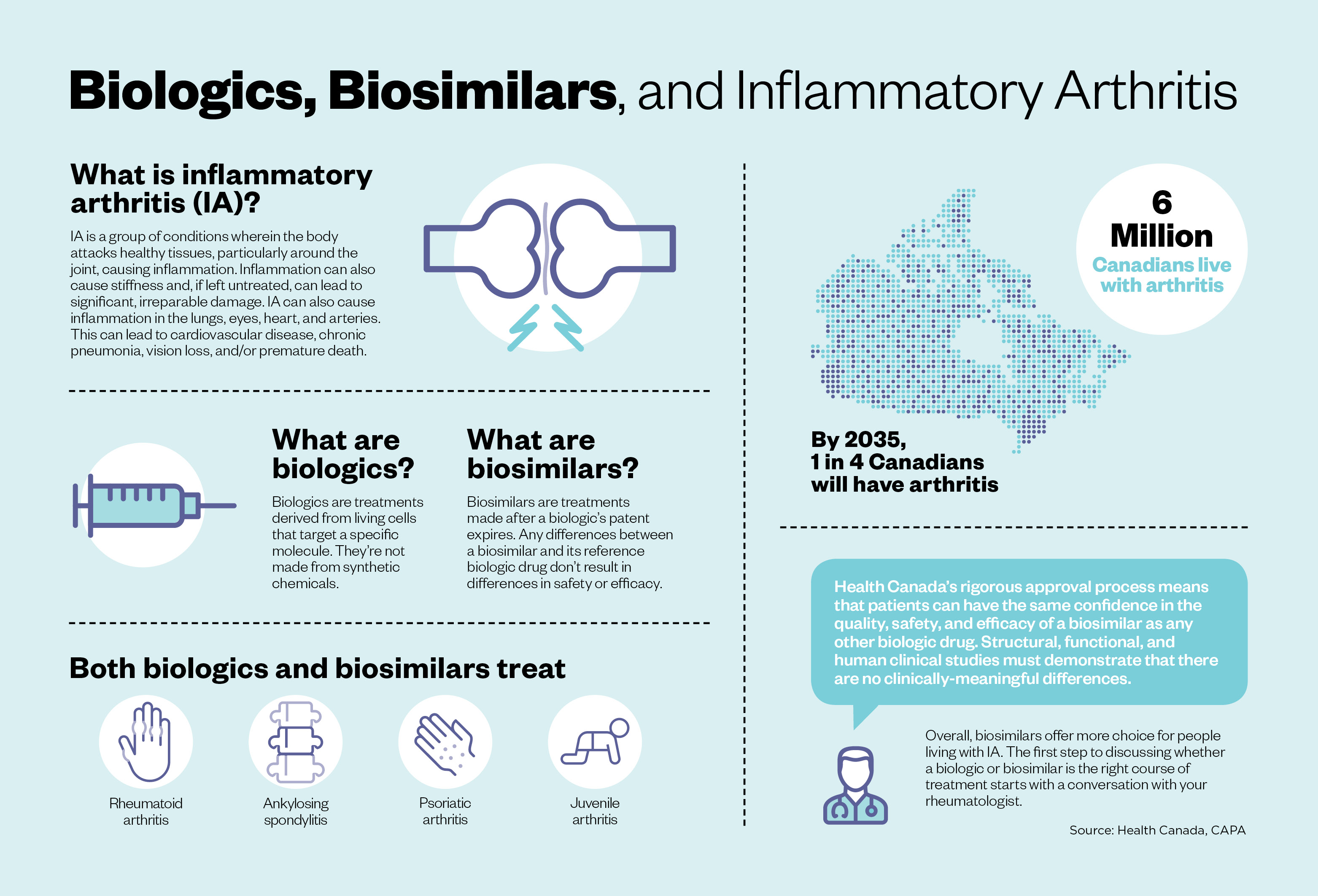
Drugs derived from complex biological sources, known as biologics, have been in use for over a century. With advances in biotechnology, the field has exploded and significantly improved the lives of patients with cancer, diabetes, arthritis and inflammatory bowel disease (IBD). As patents on some biologics expire, pharmaceutical companies are bringing their own, less costly versions of these treatments, known as biosimilars, to market.
Different but equivalent
Biosimilars aren’t new. Health Canada has approved 18 biosimilars for use by Canadian patients since 2014. Biosimilars, by definition, aren’t perfect copies of the drugs they mimic. The standards for achieving biosimilarity, however, are very high. “The biosimilar molecules must demonstrate having the same basic protein structure, with only minor folding or side-chain differences,” says Dr. Janet Pope, a rheumatologist at St. Joseph’s Health Care and a professor of medicine at Western University.
The onus of responsibility is on drug manufacturers to demonstrate to Health Canada that any minor differences between biosimilars and the original biologic will not affect patient treatment outcomes. This rigorous approval process means that patients and health care providers can have confidence in the quality, safety and efficacy of the biosimilar as any other biologic drug. Moreover, according to the Patented Medicines Pricing Review Board, the use of biosimilars can save the Canadian health care system approximately $1.8 billion per year, which can help drug plans ensure Canadians have access to innovative medicines.
As they come to market, biosimilars are providing new options for treating a wide variety of conditions, including ulcerative colitis. “Characteristic symptoms of ulcerative colitis include rectal bleeding, reduced stool consistency, and increased frequency and urgency of bowel movements,” explains Dr. Neeraj Narula, Director of the IBD clinic at McMaster University. “Biologics have changed the landscape of ulcerative colitis and are very effective therapies. Biosimilars are effective and they work in the same fashion as the originator molecule, so I don’t have concerns when using biosimilars for patients in need of biologic therapy.”
More choices, better outcomes
Biologics have proven to be very effective in managing severe cases of rheumatoid arthritis, and some of the first biosimilars approved in Canada were indicated for arthritis. As a result, rheumatologists have been on the front lines of patient concerns about switching.
“There was a time when the public and some physicians didn’t understand that generics would save a lot of money without putting someone at risk,” says Dr. John Esdaile, Scientific Director of Arthritis Research Canada. “Those on a chronic prescription for a drug often don’t notice they are being switched back and forth among the generics. No one thinks much about this anymore. The main difference today is that the injection system to administer a biosimilar is different from the originator’s. In the future, we will talk of biosimilars and no one will care. Both the rheumatologist and their pharmacist will be knowledgeable about the topic and help their patient make the transition to a biosimilar.” Biosimilars are expanding the breadth of treatments available to patients and health providers in rheumatology, IBD, and many others, but there remains a need for public education. It’s essential that patients taking or considering biologics have an informed dialogue with their doctors about biosimilars and how they can fit into their personalized treatment plans.
This article was brought to you by a leading research-based pharmaceutical company.


