April Gamache
CEO, Canadian Addiction Treatment Centres
Polarizing debates are weakening our collective strength in saving lives threatened by fentanyl.
There is no one way to solve a problem as huge and complex as the opioid crisis in Canada. Across the healthcare spectrum, heated debates are raging over how to best save lives: Is safer supply truly safe? Which approach to care is the “right one”? How should public funding be best spent?
Rather than focusing on our own individual part of the problem, it is essential that we keep our focus where it needs to be: squarely on the people we all serve.
7 / 10 patients in treatment for opioid use disorder don’t have a family doctor. Virtual care is their lifeline to the health care they need.
The toxic illicit supply of drugs is constantly morphing in new and dangerous ways. Under the crushing weight of homelessness, food insecurity, and unsupported mental health, vulnerable Canadians are being backed into a corner—one from which drugs can seem like the only escape. Keeping quality care for substance use disorder fast and easily accessible is our only hope of breaking the cycle of addiction — and we simply can’t do it in silos.

We provide same-day access to fully-integrated care at over 80 treatment centres, 365 days a year; often in isolated remote areas. For years, due to an absence of qualified local addictions specialists, our patients there have depended on virtual care to connect with doctors hundreds of kilometres away. Where there’s no road access, the medications critical to their recovery are air-dropped by plane to the clinics through our connected pharmacy shipping network. Many rural treatment centres providing lifesaving care in underserved communities are bearing the brunt of unprecedented inflation and, in many cases, are one human resource challenge away from having to close their doors. That would mean hundreds of at-risk people suddenly left without a viable option to avoid a potentially fatal accidental overdose. We can all agree that ensuring continuity of this care is critical.
If the pandemic taught us anything it’s that, in times of crisis, we need to come together. Our more than 15,000 patients deserve the best possible care. As a highly specialized branch of health care, public funding for addictions medicine is complex and precarious—one seemingly small change in funding can have unintentionally catastrophic effects on our ability to keep clinic doors open where they’re needed most. As Canada’s largest provider of evidence-based care for substance use disorder, we remain steadfast in our commitment to work with Government, health care providers and other community partners across the spectrum of care to implement innovative solutions toward achieving the goal we collectively share: saving lives.We may not know what the next toxic drug hitting the streets will look like but we do know that, in the fight to defend our communities, we’re stronger together.
Research shows that people who receive treatment for opioid use disorder in a fully-integrated care model* are
4x
more likely to stay in recovery.
IN RECOVERY
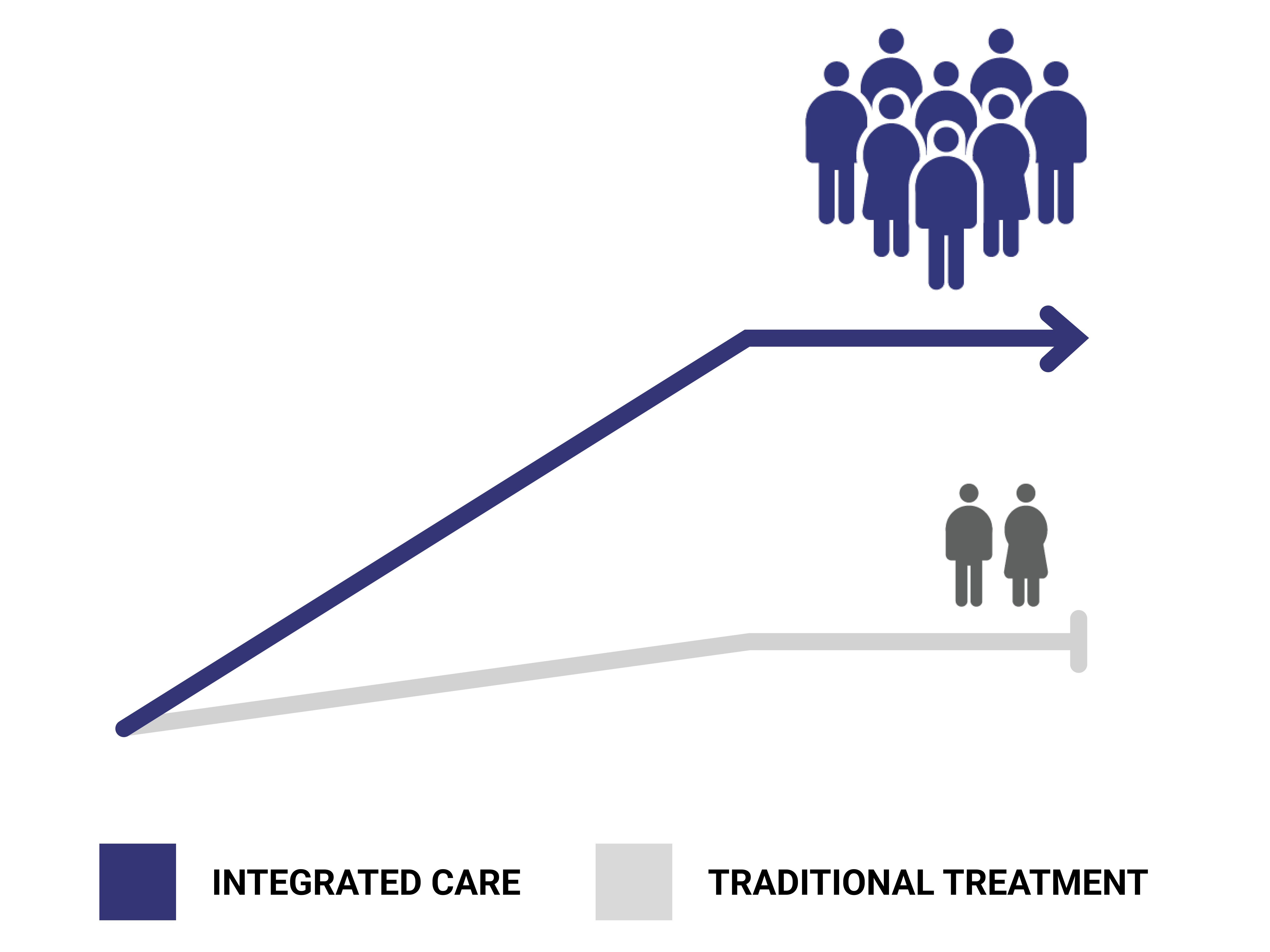
*Including onsite pharmacy services, harm reduction, regular health assessments and linkage to primary care.
*Northern Ontario School of Medicine
To learn more, visit canatc.ca.