
Antonella Pucci
Manager, Immunization Initiatives,
Canadian Public Health Association
Antonella Pucci from the Canadian Public Health Association shares her insights on the critical role of vaccines in protecting public health, addressing common misconceptions, and ensuring equitable access for all Canadians.

Why are vaccinations important for public health, and how do they help protect individuals and communities?
Vaccinations matter! They are one of the most effective public health interventions of our time, responsible for preventing millions of illnesses, hospitalizations, and deaths worldwide. Vaccines not only protect us as individuals from preventable diseases but also protect the communities we live in. This is achieved through community immunity (also known as herd immunity)—when enough people within a population are immunized against a contagious disease, it helps safeguard those who cannot be vaccinated, such as newborns or individuals with certain medical conditions.

Ironically, the success of immunization programs can make their impact less visible—when vaccines work and enough people are protected, we don’t see the cases of the diseases they prevent, leading to a false sense of security. It’s only when vaccine uptake declines that we witness the resurgence of previously controlled or eradicated diseases, such as measles. These outbreaks remind us just how important vaccines truly are.
That’s why this year, Immunize Canada’s theme for National Immunization Awareness Week is: “Don’t let history repeat itself. Protect your future. Get immunized.” Learn more and find out how to get involved [here].

Why is it important for both children and adults to stay up to date with their vaccinations?
As the immunity we receive from vaccines can wane over time, and as new vaccine developments emerge, it is essential for both children and adults to stay up to date with their vaccinations. There’s often a misconception that vaccines are just for kids—but that couldn’t be further from the truth. Vaccines are important for everyone, at every age, throughout the life course.
For children, vaccines help build early immunity to protect them against serious diseases such as measles, pertussis (whooping cough), and polio. The need for protection continues into adolescence, with important vaccines like those for meningitis, HPV, and hepatitis B. Adults need protection too—vaccines help maintain immunity, particularly against both seasonal and non-seasonal communicable diseases such as influenza, pneumonia, COVID-19, RSV, and shingles. Staying up to date with recommended immunizations throughout the life course helps prevent outbreaks, reduces pressure on healthcare systems, and ensures we continue to protect our communities for generations to come.
Talk to your doctor, nurse, pharmacist, or local public health office about getting up to date on your immunizations because it is never too late!

Can you explain how vaccines work with our immune system to prevent diseases?
Certainly! In simple terms, a vaccine contains the same antigens—or substances, such as a bacteria or virus that triggers your immune system to produce a protective immune response—that cause a specific disease, but in a form that is either killed or significantly weakened. Vaccines work by training your immune system to recognize and fight off the real disease if it’s encountered in the future.
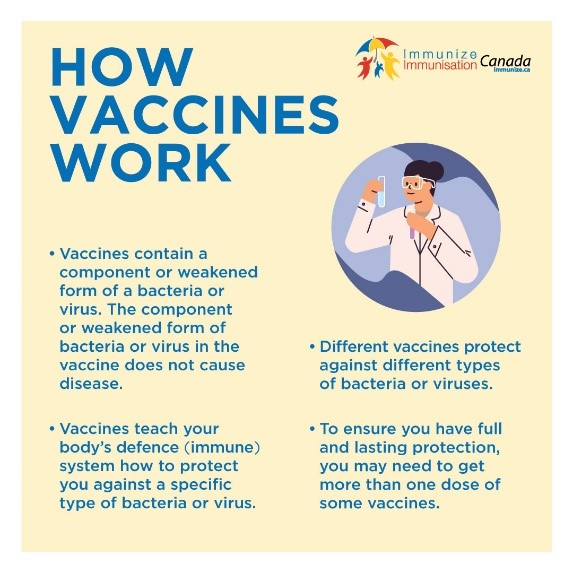
This way, immunity is achieved without people having to go through the illness itself and face potentially serious, even life-threatening, complications.
Immunization also helps the body create memory immune cells that specialize in preventing reinfection. However, as mentioned earlier, it’s important to stay up to date on all recommended vaccines to ensure you maintain protection throughout your life. Learn more about how vaccines work [here].

What are the most common misconceptions about vaccines, and how can they be addressed to improve vaccine confidence?
Unfortunately, misinformation and disinformation continue to hinder vaccine efforts, as false claims about the safety and effectiveness of vaccines circulate widely—particularly online. Common misconceptions include statements such as “Vaccines aren’t safe,” “Vaccines cause the diseases they’re meant to prevent,” and perhaps most notably, “Vaccines cause autism.” This challenge is made worse by some individuals in positions of power who spread disinformation at alarming rates, further eroding public trust. Although these claims are false and unsupported by scientific evidence, they can become deeply ingrained within social circles, leading to growing skepticism and fear around vaccination. In fact, as vaccine misinformation spreads across social media and other platforms, we’re now witnessing one of the largest measles outbreaks in years here in Canada.
While there are various strategies to counter these myths, one of the most effective approaches is education. Addressing vaccine misconceptions with compassion and empathy—while using plain, accessible language to share evidence-based information—can make a meaningful difference.

That said, providing reliable and trustworthy information is not a one-time effort; it requires ongoing engagement and a commitment to building trust within communities. Once that trust is established, it becomes easier to talk about the importance of vaccination and to promote media literacy, helping people identify and reject vaccine misinformation online. You can help us debunk vaccine misinformation by sharing our Myth-busting Mondays Series [here].

How can Canada continue to improve vaccination rates and ensure equitable access to vaccines for all populations?
As previously mentioned, stronger education and trust-building are key components in improving vaccination rates in Canada. However, these strategies alone are not sufficient to ensure equitable access or to effectively get vaccines into arms. Many barriers extend beyond vaccine hesitancy and are rooted in systemic inequities and logistical challenges.
For example, Immunize Canada led an HPV Vaccine Task Force in Ontario—which you can learn more about [here]—with the goal of increasing vaccine uptake in the province. Through our work, healthcare professionals identified a range of barriers that contribute to lower HPV vaccination rates, including:
- Needle phobia, which presents a significant psychological barrier for many individuals.
- Apathy or stigma, such as the perception that the vaccine is unimportant or the mischaracterization of the HPV vaccine as “just a sex vaccine.”
- Religious or cultural beliefs that may conflict with vaccination practices or public health recommendations.
- Challenges in patient communication, particularly when discussing the HPV vaccine, addressing misinformation, and engaging with parents who hold predetermined views.
- Time constraints and limited feasibility, as healthcare providers often have only 10–15 minutes per patient, making it difficult to prioritize immunization discussions during routine medical visits.
- Restricted access to vaccination services, due to regulatory limitations—for instance, pharmacists are only permitted to administer certain vaccines, which limits convenience and accessibility.
- Lack of a national vaccine registry, which hinders the ability of healthcare professionals to track, store, and coordinate vaccination records across different providers and jurisdictions. Immunize Canada is currently preparing a report and webinar to share these findings in more detail.
Importantly, the challenges identified by the Task Force are not limited to HPV vaccination—they reflect broader issues affecting uptake of other vaccines as well. Addressing these barriers requires coordinated, multisectoral efforts. Some key strategies include:
- Providing culturally appropriate outreach, such as developing multilingual and culturally sensitive educational materials that address specific concerns and misinformation.
- Partnering with community leaders and organizations in Indigenous, racialized, immigrant, and rural communities to build trust and promote vaccine education.
- Expanding access points by increasing the availability of vaccines in pharmacies, primary care settings, and remote areas.
- Establishing community-based clinics, such as mobile and pop-up sites in schools, workplaces, religious institutions, and other accessible community hubs.
- Offering transportation assistance, including free or subsidized rides to vaccination sites, especially in rural or underserved communities.
- Implementing digital reminders and booking tools to reduce missed appointments and improve convenience through SMS/email notifications and user-friendly scheduling platforms.
Together, these strategies can help ensure a more equitable and effective vaccine rollout across the country, addressing not only hesitancy but the broader systemic barriers that prevent individuals from accessing life-saving immunizations. Don’t let history repeat itself. Protect your future. Get immunized.
Learn more about Immunize Canada at immunize.ca.


